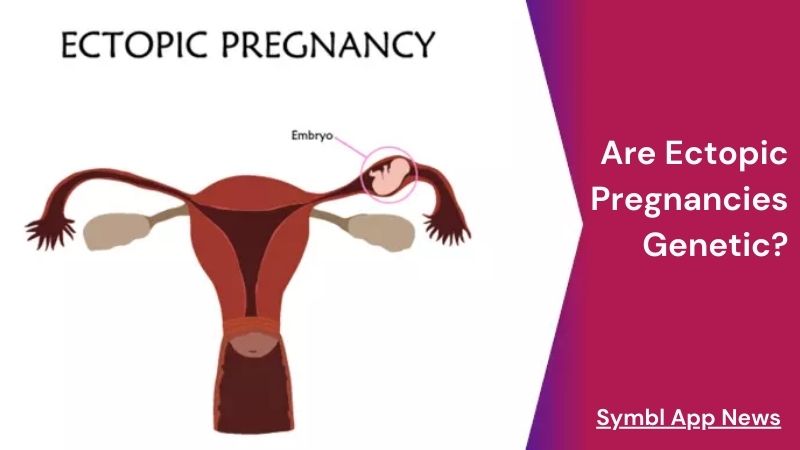
Ectopic pregnancies, though less common than intrauterine pregnancies, present a significant medical challenge, often requiring prompt intervention to prevent serious complications. These pregnancies occur when a fertilized egg implants itself outside the uterus, typically in the fallopian tubes. While numerous risk factors have been identified, including prior tubal surgery, pelvic inflammatory disease (PID), and smoking, a fundamental question persists: are ectopic pregnancies genetic? Delving deeper with Symbl.app into this query unveils a complex interplay of genetic and environmental factors shaping the susceptibility to ectopic pregnancies.
Exploring Genetic Influences:
Addressing this inquiry necessitates a comprehensive exploration of the genetic elements potentially implicated in the onset of ectopic pregnancies. Although ectopic pregnancies are not typically categorized as exclusively genetic disorders, genetic factors can indirectly impact a woman’s predisposition to such pregnancies. These genetic influences may encompass variations in genes governing reproductive organ development, hormonal regulation, or tubal function, among others. Understanding the nuanced interplay between genetic predispositions and environmental factors is crucial for discerning the complex etiology of ectopic pregnancies and devising targeted interventions to mitigate associated risks and optimize reproductive health outcomes.
1. Genetic Predisposition to Reproductive Health Conditions:
Specific genetic conditions or mutations might predispose individuals to reproductive health complications like endometriosis or pelvic inflammatory disease (PID). These conditions, marked by anomalies in reproductive organs or inflammatory responses, heighten the chances of ectopic pregnancies. Therefore, although not inherently genetic, certain genetic factors may elevate susceptibility to conditions that can culminate in ectopic pregnancies. Understanding these potential genetic predispositions can aid in proactive measures and informed decision-making regarding reproductive health and family planning, empowering individuals to mitigate risks and optimize their overall well-being.

2. Familial Patterns and Ectopic Pregnancy Risk:
Analyzing familial patterns can unveil potential genetic influences on ectopic pregnancies. Research indicates that women with a familial history of reproductive health disorders, like endometriosis or PID, might face an increased risk of ectopic pregnancies. These observed familial associations underscore a probable genetic predisposition to specific reproductive health conditions, thereby augmenting the likelihood of ectopic pregnancies. Recognizing these familial connections facilitates a deeper understanding of the genetic underpinnings of ectopic pregnancies, prompting proactive measures for risk management and informed decision-making regarding reproductive health interventions and family planning strategies.

3. Genetic Variants and Tubal Function:
The functionality of the fallopian tubes stands as a pivotal determinant in the incidence of ectopic pregnancies. Genetic variants that influence tubal function, including alterations in genes governing tubal motility or the structure of cilia lining the tubes, may potentially facilitate embryo implantation outside the uterus. Although ongoing research delves into this realm, pinpointing precise genetic variations linked to tubal function could yield valuable revelations concerning the genetic foundations of ectopic pregnancies. Such insights hold promise in elucidating the intricate mechanisms underlying ectopic pregnancies, guiding future research endeavors and informing clinical interventions aimed at mitigating associated risks and improving reproductive health outcomes.

4. Interplay of Genetic and Environmental Factors:
While genetics may contribute to the likelihood of ectopic pregnancies, it’s essential to acknowledge that other factors also play significant roles. Environmental influences, including smoking, sexually transmitted infections, and reproductive interventions like assisted reproductive technologies, can interact with genetic predispositions to elevate the risk of ectopic pregnancies. Consequently, the occurrence of ectopic pregnancies often arises from a complex interplay between genetic susceptibilities and environmental triggers. Understanding these multifaceted interactions is crucial for comprehensively assessing and addressing the risk factors associated with ectopic pregnancies, facilitating informed decision-making and targeted interventions to optimize reproductive health outcomes.
Clinical Implications and Future Directions:
Understanding the potential genetic influences on ectopic pregnancies has significant implications for clinical practice and research endeavors. Healthcare providers can incorporate knowledge of genetic predispositions into risk assessment and counseling for women of reproductive age. Genetic testing may also play a role in identifying individuals at higher risk of experiencing ectopic pregnancies, enabling proactive interventions and personalized management strategies.
Moreover, ongoing investigation into the genetic determinants of ectopic pregnancies offers a pathway to deepen our comprehension of the underlying mechanisms and uncover novel therapeutic avenues. Collaborative endeavors involving geneticists, reproductive biologists, and clinicians are pivotal for unraveling the intricate interplay between genetics and the risk of ectopic pregnancy. By synergizing expertise across diverse disciplines, researchers can elucidate the multifaceted genetic factors contributing to ectopic pregnancies, paving the way for targeted interventions and personalized approaches to mitigate risk and improve outcomes for individuals affected by this condition.
Closing Words: Are Ectopic Pregnancies Genetic?
In conclusion, while ectopic pregnancies are not solely genetic in nature, genetic factors can contribute to an individual’s susceptibility to such pregnancies. Genetic predispositions to reproductive health conditions, familial patterns, genetic variants affecting tubal function, and the interplay of genetic and environmental factors all play roles in shaping the risk of ectopic pregnancies. By elucidating these genetic influences, we can enhance risk assessment, develop personalized management approaches, and pave the way for future advancements in the prevention and treatment of ectopic pregnancies.